Glaucoma – Awareness is the Key
It is for nothing that glaucoma is called the silent thief of sight. Currently, glaucoma is the second leading cause of irreversible but preventable blindness in the world. Glaucoma is estimated to affect 27.8 million more people by 2040 in Asia, and India and China will share the maximum burden. As per a scientific study published in 2010, glaucoma was responsible for blindness in 11.2 million people and accounted for 5.5% of total blindness, making it the leading cause of irreversible blindness in India.
What causes glaucoma?
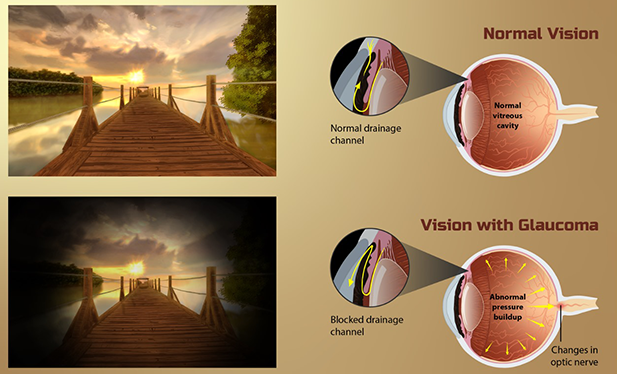
The front part of the eye is filled with a clear fluid called aqueous humor. This fluid is made in an area behind the colored part of the eye (iris). It leaves the eye through channels where the iris and cornea meet. This area is called the anterior chamber angle, or the angle. The cornea is the clear covering on the front of the eye that is in front of the iris, pupil, and angle. Anything that slows or blocks the flow of this fluid will cause pressure to build up in the eye.
The optic nerve sends visual information from the eye to the brain and is vital for good vision. Though not fully understood yet, damage to the optic nerve is often related to high pressure in the eye which leads to glaucoma. As this nerve gradually deteriorates, blind spots develop in the vision.
Risk Factors:
Increased Intraocular Pressure (IOP) is the most important risk factor for the disease, although a significant proportion of patients do not have elevated IOP.
Other risk factors include:
1. Old age, people above 55 years
2. People of non-white descent – Asians, Africans, Hispanics
3. Myopia
4. Family history of the disease
5. Systemic conditions like hypertension, diabetes, diabetes, migraines, sickle
cell anemia.
6. Eye injury or certain types of eye surgery
7. Intake of medications such as corticosteroids, anticholinergics, certain
antidepressants.
Types
The two main types of glaucoma are:
Open-angle and Angle-closure glaucoma.
There are at least eight other types which include normal-tension glaucoma,
secondary glaucoma, glaucoma in children, pigmentary glaucoma.
Signs and Symptoms
Open-angle glaucoma
1. No symptoms in early stages
2. Gradually, patchy blind spots are seen in peripheral vision (what one can see
on the side when looking ahead) first.
3. In later stages, difficulty arise in seeing things in central vision.
Acute angle-closure glaucoma
1. Severe headache
2. Severe eye pain
3. Nausea or vomiting
4. Blurred vision
5. Halos or colored rings around lights
6. Eye redness
Normal-tension glaucoma
1. No symptoms in early stages
2. Gradually, blurred vision
3. In later stages, loss of side vision
Diagnosis
Diagnostic testing to assess for glaucoma and to monitor for disease progression
primarily includes:
Tonometry - to measure intraocular pressure.
Gonioscopy - to view the angle at which the fluid drains out
of the eye and
maintains the pressure inside.
Perimetry - to evaluate their field of vision and establish the
extent of loss.
Optical coherence tomography - imaging techniques like these
give images of the
eye’s interior.
Management
The management of glaucoma is based on lowering the intraocular pressure to prevent
further optic nerve damage. Currently, there are five major classes of medications
that are used to lower the intraocular pressure: Beta-adrenergic antagonists,
adrenergic agonists, parasympathomimetics, prostaglandin-like analogues and
carbonic anhydrase inhibitors.
The goal of therapy is to maintain adequate vision for patients during their
lifetime, keeping in mind the possible adverse effects of the drugs. If additional
lowering of IOP is indicated or if medication fails to sufficiently lower the IOP,
laser trabeculoplasty is usually the next step.
If IOP is still not adequately controlled, incisional glaucoma surgery is
indicated. Use of neuroprotective agents, which directly protect the optic nerve in
glaucoma, are being evaluated in clinical trials.
Prevention
Currently, regular eye exams are the best form of prevention against significant
glaucoma damage.
High risk factor individuals should get tested every year or two after age 35.
Managing systemic conditions like diabetes, hypertension under control and prevention
of eye trauma are other measures to prevent development of glaucoma.
Challenges in catching the invisible thief of sight in India
The critical challenges in glaucoma management in India are: low levels of awareness,
undetected and undiagnosed cases, poor access to glaucoma diagnostic and therapeutic
services, and issues related to compliance with treatment. A study found that
two-thirds of glaucoma patients did not avail locally available dedicated eyecare
services, due to financial, logistic, and social reasons.
Given the dire necessity to screen Indian population, particularly from rural regions, who are genealogically more predisposed to developing glaucoma, awareness is the key to preventing the clinical, economic and lifestyle burden of vision loss due to glaucoma.
Therefore, there is an emerging need to address the challenge of glaucoma management as a public health problem at different levels targeting the public, service care providers, and the eye healthcare system.
World Glaucoma Week being celebrated from Mar10 -16, 2024, aims to raise awareness about glaucoma globally. It includes activities alerting people to have regular eye and optic nerve checks to detect glaucoma earlier, thus preserving sight. This year’s theme is Uniting for a Glaucoma-Free World.
Sachetana Eye Clinic joins the campaign to raise awareness on glaucoma and its care. Call or visit Sachetana to know more and participate in the campaign.
08023289111/333/9036339111. Or visit www.sachetanaeyeclinic.com for appointments.


